Most men are choosing a radioactive seed implant for treatment of their prostate cancer due to its superior
long-term results and lack of long-term side effects. Recently published studies have shown that with 15 years of follow-up,
a seed implant is a very effective treatment for prostate cancer. If found early, more than nine out of ten men will be cured
of their cancer after seed implants.
Prostate seed implantation is based upon the use of tiny radioactive seeds, each smaller than a grain of rice. The seeds
are made of titanium and contain a small amount of palladium or iodine. After placement, the seeds emit an intense amount
of radiation to the cancer in the prostate, and only minimal radiation outside the prostate to other areas, such as the bladder
and rectum. The seeds give off radiation for a few months and then are permanently inactive. Because cancer cells are much
more sensitive to radiation than normal cells, they can be selectively killed.
Prostate implantation is a simple outpatient procedure that takes less than one hour. Men typically report to the hospital
in the morning, and return home a few hours later. The entire procedure is done through very thin needles while under a light
general or spinal anesthetic. There is no cutting involved and no stitches are required. With an ultrasound in the rectum,
a live picture of the prostate is obtained. The Urologist then precisely places the needles in the prostate, through the perineum
(the area of skin between the scrotum and rectum). The Radiation Oncologist then inserts the seeds through the needles. Once
the procedure is completed and the anesthesia has worn off, you can go home. Most men do not complain of any pain and most
do not need a catheter after the procedure. Unlike surgery, the risk of incontinence is less than 1%. Most men return to their
normal activities that next morning, and can return to work, playing golf, etc.
For more information about the seed implant procedure, please click here
↑ BACK TO TOP
..............................................................................................................................................................
Surgery - Prostatectomy
The only other treatment besides seed implants and radiation therapy proven to cure prostate cancer is a prostatectomy.
This is considered a major operation that typically takes several hours. It involves making at least a 4” incision in the
lower abdomen to surgically remove the prostate gland. Hospitalization is required for a few days, and a catheter in the bladder
needs to be used in all patients for a few weeks following the procedure.
Robotic prostatectomy can be done at select institutions. Here, the surgeon guides robotic arms to perform the operation.
Smaller incisions are used resulting in somewhat shorter recovery times. Some studies have questioned whether there is a higher
risk of positive margins (leaving cancer behind) following robotic surgery. Long-term side effects are similar to open prostatectomy
in most studies. Loss of urinary control (incontinence) and loss of sexual function (impotence) can occur with this procedure.
The likelihood of these complications varies greatly with the skill and experience of the surgeon.
A prostatectomy can only cure men when the cancer is completely removed. If surgery leaves behind even a few microscopic
cancer cells, these can later grow and ultimately spread.
Robotic prostatectomy can be done at select institutions. The surgeon guides robotic arms to help perform the operation.
Smaller incisions are used, which may result in slightly shorter recovery times. Some studies have shown a higher risk of
positive margins (leaving cancer behind) following robotic surgery requiring supplemental treatment afterwards. (JCO 2008) A recent major study from Harvard showed that men who underwent robotic surgery actually had higher rates of incontinence
(loss of urinary control) and loss of sexual function (impotence) than men treated with an open prostatectomy (JAMA 2009) (Eur Urol 2010). The likelihood of these complications, as well as success rates, varies greatly with the skill and experience of the
surgeon. Several recent studies have shown that outcomes following surgery are significantly worse if the surgeon has performed
less than 250 of these procedures. (JNCI 2007) (NEJM 2002)
↑ BACK TO TOP
..............................................................................................................................................................
IGRT and IMRT
Patients with more aggressive or advanced stages of cancer have a higher than ideal risk of cancer outside the prostate.
This is an area beyond the surgeon’s reach. External radiation delivered from a high-energy X-ray machine called a linear
accelerator can help treat just outside the prostate, where the prostate cancer cells may reside. Using the latest computer
technology, the prostate can be precisely targeted within the body, and radiation can be safely delivered.
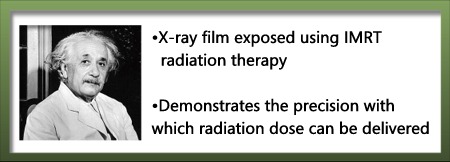
Image Guided Radiation Therapy (IGRT) takes IMRT one step further. To accomplish this, we use various technologies such
as BAT ® ultrasound imaging, Acculoc ® tracking of implanted fiducials, or Cone-beam ® CT scans before each daily treatment,
to acquire an image of the prostate and surrounding anatomy. The goal is to detect any slight change in position of the prostate
gland that may result from movement or variations in filling of the bladder or rectum. Using this information, the computer
adjusts the radiation beam accordingly in order to precisely target the treatment to your prostate’s position that day. It
is the latest and most advanced system for the delivery of radiation, allowing much greater precision than proton therapy.
This allows us to further maximize the radiation does to the prostate and minimize the dose to the surrounding normal organs.
 Prior to beginning this treatment, our patients undergo a CT scan of the pelvis in the Radiation Oncology department. This
scan is used to create a customized plan, tailored to fit each patient’s anatomy precisely. The IGRT is typically given for
only a few minutes a day, five days a week. When combined with a seed implant, this part of the treatment is approximately
five weeks long. If given alone, without a seed implant, the treatment is typically for eight weeks. Prior to beginning this treatment, our patients undergo a CT scan of the pelvis in the Radiation Oncology department. This
scan is used to create a customized plan, tailored to fit each patient’s anatomy precisely. The IGRT is typically given for
only a few minutes a day, five days a week. When combined with a seed implant, this part of the treatment is approximately
five weeks long. If given alone, without a seed implant, the treatment is typically for eight weeks.
Radiation treatment is completely painless and non-invasive. During treatment, the most commonly reported side effects
are slight fatigue and having to go to the bathroom more frequently. You will NOT develop any nausea, abdominal pain, hair
loss, or skin burning. You will NOT lose your ability to control your bowels or bladder. You will be able to continue working
full-time and should enjoy all of your regular activities.
↑ BACK TO TOP
..............................................................................................................................................................
Case for Combined Treatment
For treatment to be effective in patients who have more aggressive or advanced stages of prostate cancer, it must be directed
at both the prostate and the surrounding areas where cancer cells may have spread. To accomplish this, a prostate seed implant
is typically combined with a few weeks of external radiation and/or a temporary hormone blocking medicine to actually give
cure rates similar to those seen in patients seen with early stages of cancer.
The seed implant delivers a high dose of radiation to the prostate, where most or all of the cancer cells reside. It gives minimal radiation
to the surrounding areas. The hormone therapy and IGRT (external radiation) not only treat the cancer in the prostate, they also attack cancer cells that may have spread
outside the prostate.
IGRT (or intensity modulated radiation therapy) delivered from a high-energy linear accelerator can help treat just outside
the prostate, where the prostate cancer cells may reside. IGRT is the latest and most advanced system for the delivery of
external radiation. This technique allows for maximum radiation to be delivered to the prostate and the surrounding areas
at risk for harboring cancer cells, while minimizing radiation to the normal areas, such as the bladder and rectum. When combined
with a seed implant, this part of the treatment is typically a few minutes a day, five days a week, for five weeks.
The radiation treatment is completely painless and non-invasive. During treatment, the most commonly reported side effects
are slight fatigue and having to go to the bathroom more frequently. You should NOT develop any nausea, abdominal pain or
loss of hair on your head. You will NOT lose your ability to control your bowels or bladder. You will be able to continue
working full-time and should enjoy all of your regular activities.
Hormone Blocking Therapy
Prostate cancer typically feeds on testosterone, the male hormone. A combination of a shot (Lupron or Zoladex) that you
receive every few months from your Urologist, and pills (Flutamide or Casodex) that you take daily can temporarily block all
of the testosterone in your body. By cutting off the “food supply” to the cancer, several helpful things happen:
- After a few months, your prostate will shrink 30-40% in size. In men with large prostate glands, it becomes easier to
distribute the seeds for the implant and fewer seeds are required. An added bonus is that you will probably notice that it
is easier to urinate because your prostate is smaller.
- Some cancer cells outside the prostate may actually die, or “starve to death.”
- The remaining cancer cells can be made more sensitive or vulnerable to the upcoming radiation and thus more likely to
be killed.
While hormone-blocking treatment alone will not permanently rid the body of the cancer, it has been shown to improve cure
rates with radiation in men with more advanced stage cancer. It also has the ability to make the seed implant procedure possible
in men with very large prostates that would have otherwise been technically too difficult to implant. When administered, men
typically take the hormone blocking treatment for two to three months before beginning radiation, and continue the treatment
until after the seed implant. Common side effects from the hormone blockers include temporary hot flashes, fatigue, and loss
of libido.
↑ BACK TO TOP
..............................................................................................................................................................
Proton Beam Cancer TreatmentProton beam radiation is an older technology that has actually been in use since the 1950s. Rather than treating cancer with
photons, as occurs with IGRT, men are simply treated with a different type of radioactive particle, called protons. Some men
have been interested in comparing proton beam to newer and more precise forms of treatment, such as prostate Seed Implants and IGRT. The safety and effectiveness of seed implants and IGRT has been thoroughly studied in hundreds of scientific papers,
with superb long-term 15 year outcomes. In contrast, after 50 years of proton use, there is still remarkably very little published
data on its cure rates and complications. There are no studies reporting outcomes beyond 5 years after treatment with proton
beam. There are no studies showing long-term potency and incontinence rates. This data is critical for men with a long life
expectancy. A review of every published study on proton beam radiation shows that patients suffer 20-40% higher cancer recurrence
rates, are more likely to develop long term complications, and are at a greater risk of developing new cancers than those
treated with seed implants. In addition, proton beam therapy is very time consuming (9 weeks of daily treatment are required),
costly (more than $100,000), and not covered by many insurance plans. For these reasons, most major cancer centers throughout
the world have decided not to pursue the less effective proton beam technology and instead have focused their attentions on
more innovative and successful seed implant and IGRT programs for the optimal treatment of prostate cancer.
↑ BACK TO TOP
..............................................................................................................................................................
CyberKnife
CyberKnife is a trademarked name for a machine designed to deliver stereotactic body and head radiosurgery. It consists
of a linear accelerator mounted onto a robotic arm. It can deliver small pencil thin beams of radiation. Radiosurgery typically
involves treatment of very small areas of tissue. Radiosurgery , as well as the CyberKnife were first developed exclusively
to treat small brain tumors and other abnormalities of the brain. Radiosurgery to the brain can now be delivered using machines
such as Gamma knife, and Linear accelerator based radiosurgery. With current linear accelerator technology, all of these systems
are relatively equivalent in their ability to deliver precise radiation treatment to small areas and limit dose to surrounding
normal brain tissue. The CyberKnife has recently been used to treat prostate cancer. It involves treating the prostate with
5 fractions of high dose radiation. Although it has been marketed as a unique form of radiation, it is not. It is a form of
hypofractionated photon beam radiation therapy. Hypofractionation means delivering radiation therapy in a shorter period of
time with fewer than standard number of fractions using relatively high doses per fraction. For example hypofractionated radiation
for prostate cancer using the CyberKnife usually involves treating with dose fractions of 700 or 800 cGy for a total of five
fractions. This is in contrast to standard radiation which usually involves doses of 180 to 200 cGy per fraction given for
a total of 45 fractions. Hypofractionated radiation can be delivered using the CyberKnife, as well as commonly available linear
accelerators that employ intensity modulated radiation therapy (IMRT) as well as image guided radiotherapy (IGRT). The CyberKnife
offers no advantage over these more commonly available treatment machines.
↑ BACK TO TOP
..............................................................................................................................................................
Retro-Pubic Radical Prostatectomy
This is an operation used to remove the prostate gland from the body in order to treat men with prostate cancer. It involves
making an incision in the skin between the umbilicus (belly button) and the pubic bone. The surgeon enters the space behind
the pubic bone (hence the name retro-pubic). The surgery is known as an extra-peritoneal operation because the surgeon operates
outside of the peritoneal reflection which is a membrane that holds the abdominal contents. The prostate is cut away from
the bladder. The bladder neck (end of the bladder) is dissected away from the prostate. The prostate is also cut away from
its attachment to the urethra, just above the uro-gentital diaphragm (pelvic floor muscles or external sphincter). The bladder
neck is then re-anastomosed (re-attached) to the urethra and the prostate is removed from the body along with the attached
seminal vesicles. A small margin of normal surrounding tissue is removed as well. The main limitation of this operation from
a cancer stand point is that, due to the prostate close proximity to the bladder , rectum and external sphincter, adequate
normal tissue margins are often difficult to obtain. In other words, if inadequate amount of surrounding normal tissue is
removed along with the prostate, it is possible that microscopic cancer cells can be left behind. Indications that cancer
cells have been left behind can be found by examining the pathology report from the surgery. Pathologic findings of positive
surgical margins, seminal vesicle invasion, extra-capsular tumor invasion are all signs that cancerous cells may have been
left behind in the surgical bed. The major side effects of such an operation are urinary incontinence, of varying degrees,
sexual dysfunction (penile erectile problems), bladder neck contractures and penile shortening. In addition, there is a small
risk of death secondary to the procedure since it is still a major surgical operation .
↑ BACK TO TOP
..............................................................................................................................................................
|